Find your path to pelvic organ prolapse relief
No two people walk the same path to a diagnosis or solution. Every woman’s prolapse journey is different, and they may reach these steps at different paces and during different times in their lives.
Are the symptoms you’re experiencing more than just an inconvenience? Learn about the signs and causes of pelvic organ prolapse.

There are several different types of pelvic organ prolapse, with different names depending on the organs involved.
Learn more

While it is not life-threatening, women with prolapse experience symptoms that impact their day-to-day lives and keep them from experiencing moments to the fullest.
Learn more

The right doctor will listen to you and put your needs first. But how do you find them?
Find a specialist

What is prolapse?
Nearly half of all women between ages 50 and 79 have prolapse symptoms.1
Pelvic organ prolapse (POP) is the dropping of the pelvic organs caused by the loss of normal support of the vagina. It occurs when there is weakness or damage to the normal support of the pelvic floor causing pelvic organs (the vagina, cervix, uterus, bladder, urethra, intestines or rectum) to drop down. Women with POP may feel or see a bulge coming out of the opening of their vagina. 2
Experiencing pelvic organ prolapse can be challenging — it can interfere with your activities, intrude on your personal life, and cause some serious discomfort.2 However, there are effective solutions3 that can repair POP at the source, so you can get back to living the life you want.
Types of prolapse
There are several different types of pelvic organ prolapse, with different names depending on the organs involved.4
Female pelvic anatomy without prolapse
Anterior Vaginal Wall Prolapse (Cystocele)
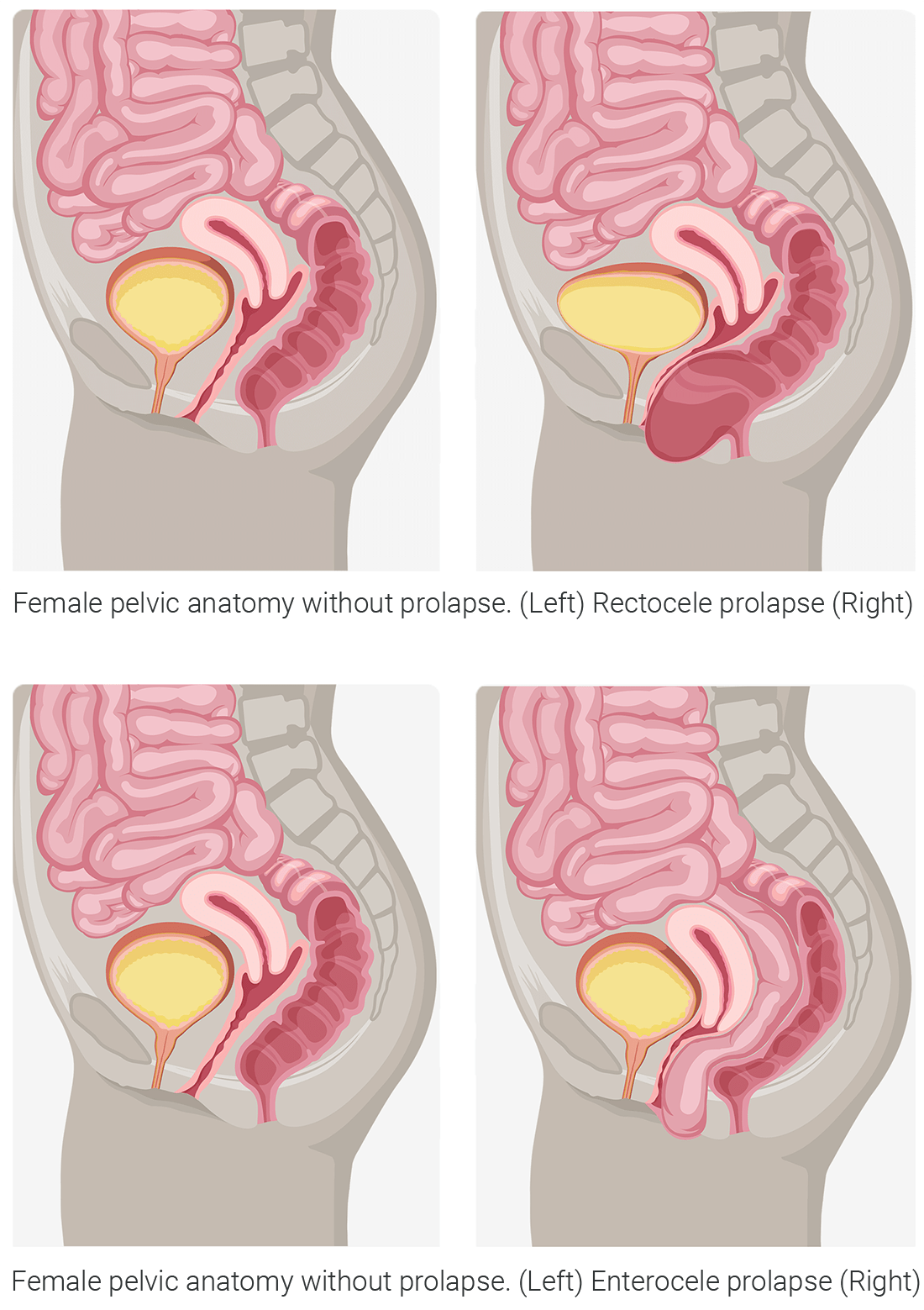
occurs when there is a loss of support to the front wall of the vagina. The bladder drops down and may cause a bulge in the vaginal opening.Posterior Wall Prolapse (Rectocele or Enterocele)
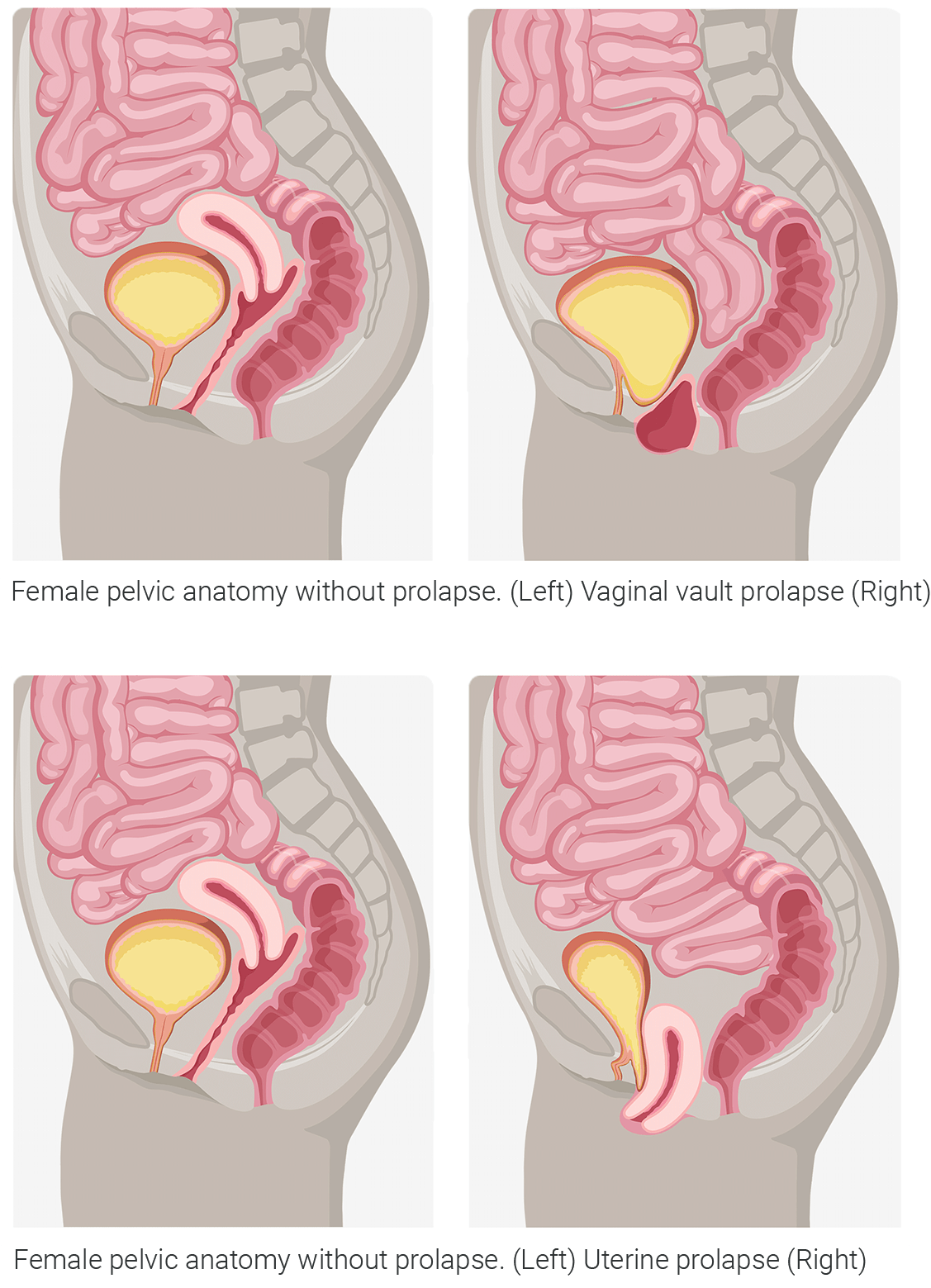
occurs when there is a loss of support to the back wall of the vagina. The rectum or intestines drops down and may cause a bulge in the vaginal opening.Apical Prolapse (Vaginal vault or Uterine)
occurs when there is a loss of support to the uterus and the top part of the vagina after a hysterectomy. These types of prolapse are often associated with the loss of anterior or posterior vaginal wall support.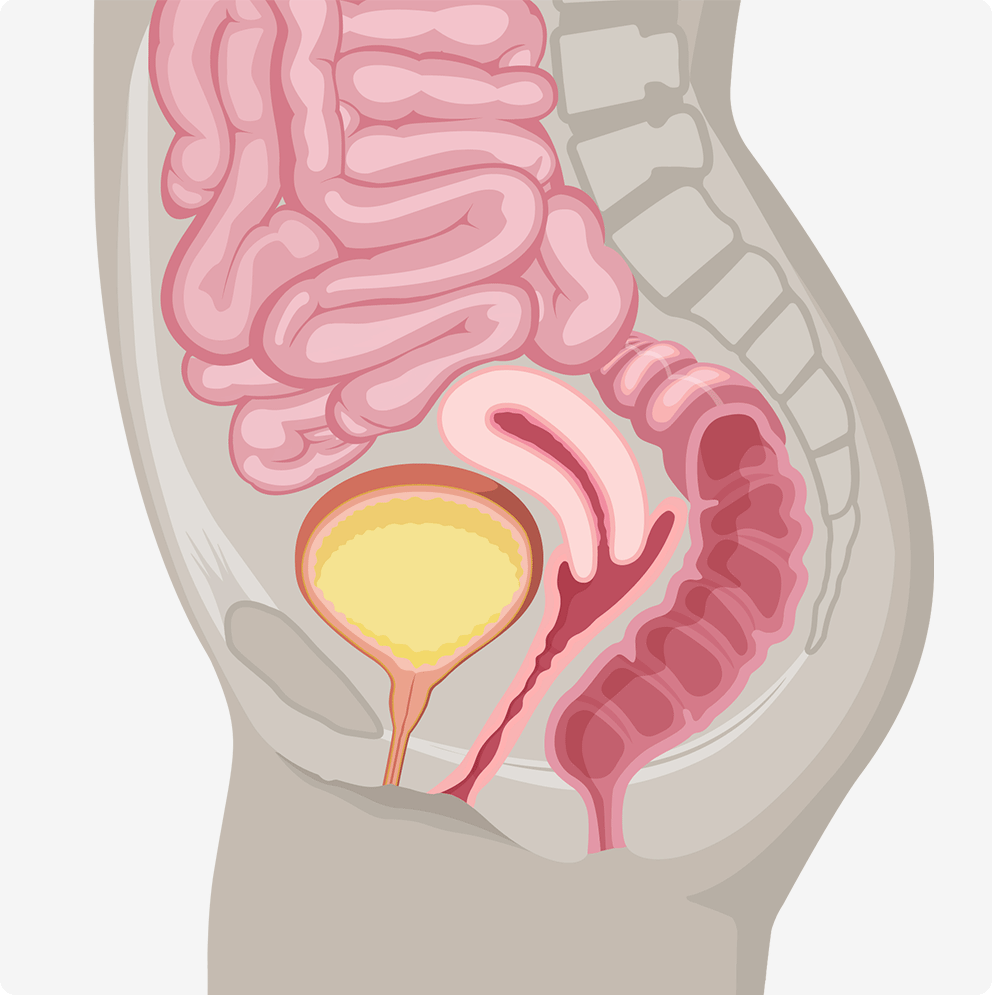
Female pelvic anatomy without prolapse
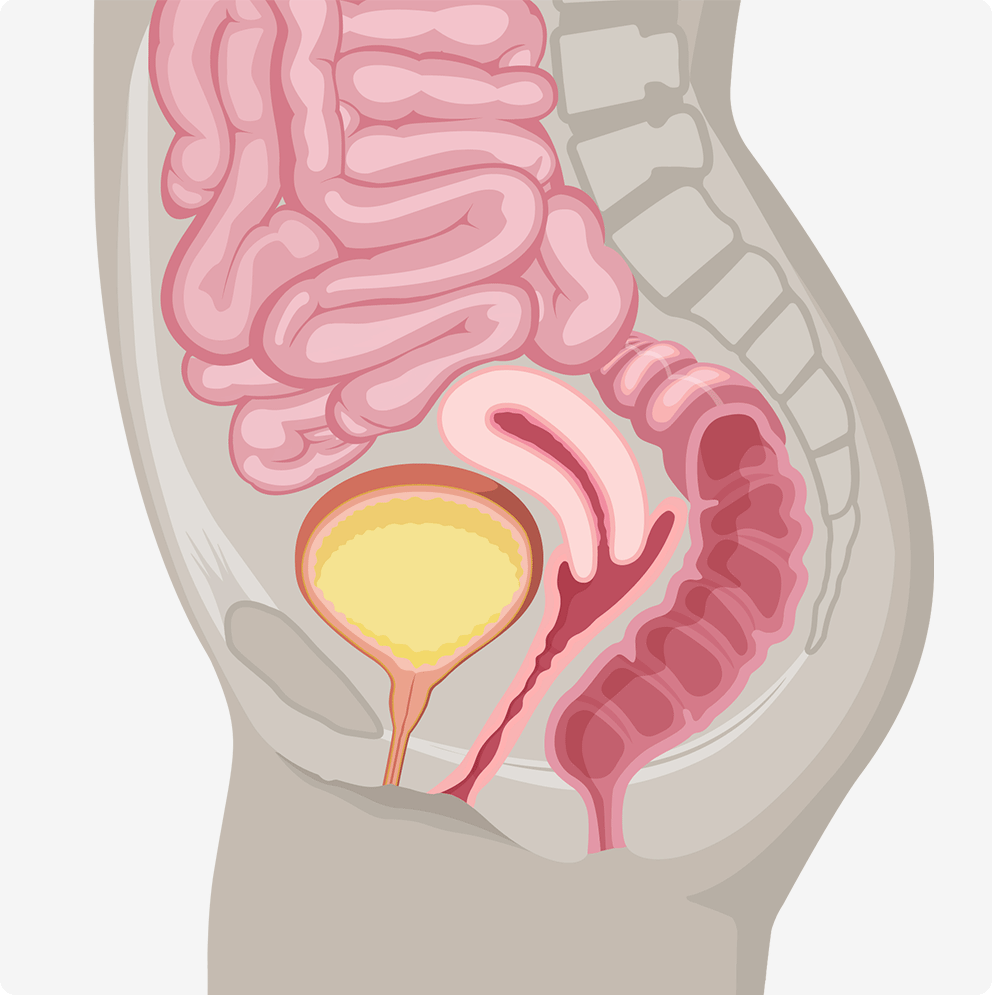 Female pelvic anatomy without prolapse
Female pelvic anatomy without prolapse
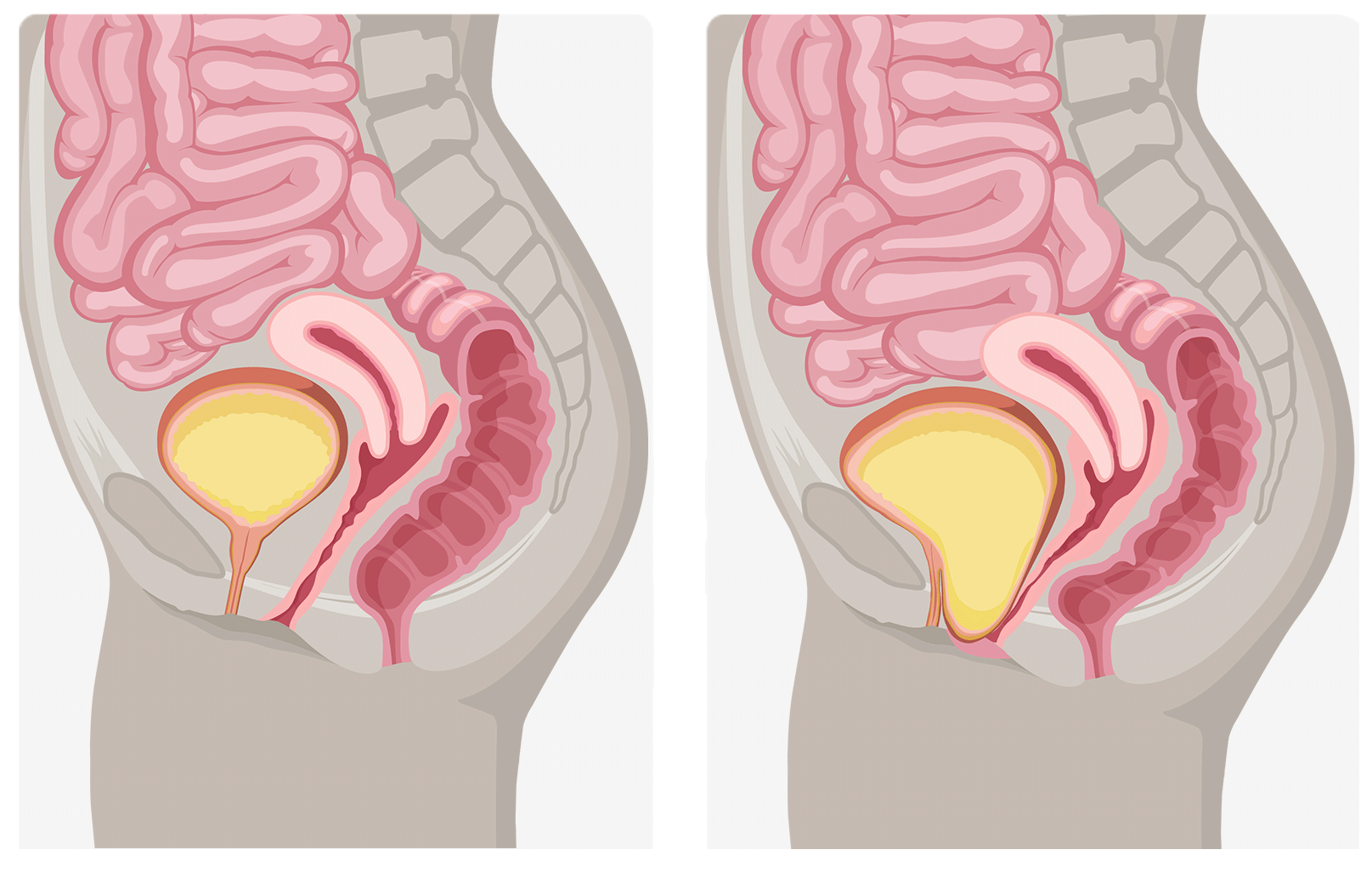 Female pelvic anatomy without prolapse. (Left) Cystocele prolapse (Right)
Female pelvic anatomy without prolapse. (Left) Cystocele prolapse (Right)
Symptoms of prolapse
While it is not life-threatening, women with prolapse experience symptoms that impact their day-to-day lives and keep them from experiencing moments to the fullest. But these symptoms won’t always seem obvious. As prolapse progresses, the symptoms may become more apparent and painful. If you are experiencing prolapse, you may feel:
- Pressure in the pelvic region, vaginal discomfort, pain or bleeding4
- Pulling or aching in the lower abdomen or pelvis, a bulge coming out of the vagina4
- Pain or discomfort during sex5
- Difficulty urinating or having a bowel movement4
Symptoms of prolapse
While it is not life-threatening, women with prolapse experience symptoms that impact their day-to-day lives and keep them from experiencing moments to the fullest. But these symptoms won’t always seem obvious. As prolapse progresses, the symptoms may become more apparent and painful. If you are experiencing prolapse, you may feel:
- Pressure in the pelvic region, vaginal discomfort, pain or bleeding4
- Pulling or aching in the lower abdomen or pelvis, a bulge coming out of the vagina4
- Pain or discomfort during sex5
- Difficulty urinating or having a bowel movement4
What causes prolapse?
Pelvic organ prolapse can drastically impact your lifestyle. Things that can cause the muscles in the pelvis to become stretched or weakened include:
- Pregnancy and childbirth2
- Genetics2
- Smoking2
- Pelvic Floor Injury2
- Chronic constipation2
- Chronic coughing2
- Obesity2
- Menopause2
- Nerve and muscle diseases2
What causes prolapse?
Pelvic organ prolapse can drastically impact your lifestyle. Things that can cause the muscles in the pelvis to become stretched or weakened include:
- Pregnancy and childbirth2
- Genetics2
- Smoking2
- Pelvic Floor Injury2
- Chronic constipation2
- Chronic coughing2
- Obesity2
- Menopause2
- Nerve and muscle diseases2

Understanding treatment options
There’s nothing simple about dealing with prolapse, but there are treatment options. Your physician may recommend some of these non-surgical options as a first step to relief:
- Vaginal pessary: a removeable device placed in the vagina to support the pelvic floor and support the prolapsed organ. Your physician will fit and insert the pessary, which must be cleaned frequently and may have to be removed before intercourse.6
- Kegels: an exercise you can do on your own or with the guidance of a pelvic floor therapist to help strengthen your pelvic floor muscles.7
- Biofeedback therapy: a technique that uses different types of devices to give information on how well pelvic muscles are contracting. This information can help improve awareness and control of pelvic floor muscles.7
Non-surgical options may involve long-term treatment, ongoing maintenance and continued expenses, and may not address the underlying condition.
Non-surgical options aren’t the only approach.
You have the option of surgical solutions backed by over 15 years of experience and clinical data with firsthand testimonials from those who’ve undergone POP procedures and experienced successful outcomes.
The type of surgery you get depends on the type of prolapse you have. Not every solution is right for every person – treatment decisions must be unique to each individual’s medical history, symptoms and lifestyle.
Finding the right doctor who will recommend the right procedure based on your needs will help make sure you’re on the right path.

What are the outcomes?
Women experiencing POP deserve a clinically proven and effective solution that lasts.
Prolapse repair procedures have effective outcomes.
0 %
of patients were “satisfied”
or “very satisfied”8
0 %
of patients stated they
would definitely “do it all over again” if they had the chance8
0 %
stated they “would definitely recommend to a friend”8
Patient spotlight
Laurie’s story
Laurie first heard the words “cystocele,” “rectocele” and “pelvic organ prolapse” before her symptoms started, during a regular annual exam with her gynecologist.

Find a specialist
Locate a pelvic surgery specialist near you

Take back your normal
Locating a doctor with the expertise and empathy to treat your condition is key. You’re probably wondering, “Is there a pelvic surgical specialist near me?” We’ve got that covered.
Simply enter your ZIP code to see a listing of pelvic doctors in your area. Each listing provides the doctor’s name and area of pelvic health expertise, along with their website, phone number and distance from your home.
This directory was created and is maintained by Coloplast. It is intended to support patients who want to learn more about treatment options for stress urinary incontinence (SUI) and pelvic organ prolapse (POP) by helping connect them to physicians who have demonstrated qualifications and interest in providing quality care for these conditions. Names and details in this directory are provided for your information only. Decisions regarding choice of physician and treatment are a patient’s responsibility, as is all communication and interaction with listed medical professionals. Any information you send to a physician is not covered by the Coloplast Privacy Policy.
Physicians listed on the Physician Locator pay no fee for inclusion. Some physicians on this list may purchase products from, provide consulting services to and/or be a party to a co-marketing agreement with Coloplast. Coloplast makes no representations or warranties regarding, and shall not be responsible for, the competencies or skill level of any of the physicians listed on the Physician Locator or the quality of their procedural outcomes. You and your physician must determine the right procedure for you.
For more information about this physician finder or if you have questions about how to add or manage directory listings please contact the administrator.
Important safety information
Pelvic organ prolapse (POP) is a condition in which the muscles of a woman’s pelvis become weak or damaged and can no longer support the pelvic organs (such as the bladder, uterus and rectum), causing them to push into the vagina. This condition can cause pain in the pelvis, discomfort while going to the bathroom and problems with having sex.
Pelvic organ prolapse can be treated with a surgical procedure in which mesh is implanted to support the pelvic organs. Restorelle® Y, Y Contour™, M, L, and XL mesh is a non-absorbable mesh that is surgically implanted through the abdomen (transabdominally) and once implanted into your body is permanent. The mesh is intended to act as a support to the weak or damaged pelvic muscles to prop up the muscles while new tissue grows into the mesh to provide strength and support, preventing the pelvic organs from pushing into the vagina. A mesh is implanted inside the abdomen to support the internal organs. The operation to place a mesh is considered major surgery.
Restorelle Y, Y Contour, M, L, and XL is indicated for use as a bridging material for sacrocolposuspension/sacrocolpopexy (transabdominal placement via laparotomy, laparoscopic, or robotic approach) where surgical treatment for vaginal vault prolapse is warranted.
Restorelle Y, Y Contour, M, L, and XL is not for females who have the following: are pregnant or desire for future pregnancy, potential for further growth (e.g., adolescents), pre-existing local or systemic infection, taking blood thinning medication (anti-coagulant therapy), any condition, including known or suspected pelvic pathology, which could compromise implant or implant placement, and sensitivity/allergy to polypropylene.
Check with your Physician on the warnings, precautions and risks associated with the use of this mesh.
The effectiveness of Restorelle Y, Y Contour, M, L, and XL has not been validated by a prospective, randomized clinical trial.
A thorough assessment of each patient should be made to determine the suitability of a synthetic mesh procedure.
Check with your Physician on:
- Alternative pelvic organ prolapse treatments that may be appropriate
- The reason for choosing transabdominal mesh
- The postoperative risks and potential complications of transabdominal mesh surgery
- The mesh to be implanted is a permanent implant
- Some complications associated with the implanted mesh may require additional surgery; repeat surgery may not resolve these complications
- Serious adverse tissue responses or infection may require removal of parts of the mesh, or the entire mesh, and complete removal of the mesh may not always be possible
- Individuals who have varying degrees of collagen laydown that may result in scarring
- Certain underlying conditions may be more susceptible to postoperative bleeding, impaired blood supply, compromised/ delayed healing, or other complications and adverse events, as with all surgical procedures
As with all surgical procedures, patients with certain underlying conditions may be more susceptible to postoperative bleeding, impaired blood supply, compromised/delayed healing, or other complications and adverse events.
The risks and benefits of using Restorelle Y, Y Contour, M, L, and XL should be considered in all patients, taking into account patients with the following underlying conditions:
- Age-related underlying conditions
- Autoimmune disease
- Coagulation disorder
- Connective tissue disorder
- Debilitated or immunocompromised state
- Diabetes
- Pelvic radiation therapy or chemotherapy
- Physical characteristics (e.g., body mass index)
- Smoking-related underlying conditions
- Urinary tract anomalies
Any future pregnancy could negate the benefits of this mesh surgical procedure. You should report any bleeding, pain, abnormal vaginal discharge or sign of infection that occur at any time.
Adverse events are known to occur with transabdominal synthetic mesh procedures and implants.
Adverse events following mesh implantation may be new onset (de novo), persistent, worsening, transient, or permanent.
Potential complications include, but are not limited to: abscess (acute or delayed), adhesion/scar formation, allergy, hypersensitivity or other immune reaction, bleeding, hemorrhage or hematoma, bowel obstruction, constipation and/or defecatory dysfunction, fecal incontinence and/or anal sphincter incompetence, ileus, dehiscence, delayed wound healing, extrusion, erosion or exposure of mesh into the vagina or other structures or organs, fistula formation, infection, inflammation (acute or chronic), local irritation, mesh migration, necrosis, new onset (de novo) and/or worsening painful intercourse (dyspareunia), neuromuscular symptoms (acute or chronic), pain (acute or chronic), partner pain and/or discomfort during intercourse, perforation or injury of soft tissue (e.g., ligaments, muscles, nerves, vessels), structures, or organs (e.g., bowel, rectum, bladder, urethra, ureters, vagina), seroma, suture erosion, bladder storage dysfunction (e.g., increased daytime frequency, urgency, nocturia, overactive bladder, urinary incontinence), ureteral obstruction, urinary tract infection, voiding symptoms (e.g., dysuria, urinary retention, incomplete emptying, straining, positional voiding, weak stream), de novo or worsening prolapse in untreated compartment, granulation tissue formation, palpable mesh (patient and/or partner), recurrent prolapse, sexual dysfunction, vaginal discharge (abnormal) and vaginal scarring, tightening, rigidity, shortening and/or contracture.
The occurrence of these events may require one or more revision surgeries, including removal of the mesh.
Complete removal of the mesh may not always be possible, and additional surgeries may not always fully correct the complications.
There may be unresolved pain with or without mesh explantation.
This treatment is prescribed by your physician. Discuss the treatment options with your physician to understand the risks and benefits of the various options to determine if mesh is right for you.
Caution: Federal law (USA) restricts this device to sale by or on the order of a physician.
Minneapolis, MN
PM-07280 02/19/2019
References:
- Barber, M. D., & Maher, C. (2013). Epidemiology and outcome assessment of pelvic organ prolapse. International urogynecology journal, 24(11), 1783–1790. https://doi.org/10.1007/s00192-013-2169-9
- (n.d.). Pelvic Organ Prolapse. Voices for PFD. Retrieved December 2, 2022 from https://www.voicesforpfd.org/pelvic-organ-prolapse/
- (n.d.). Pelvic Organ Prolapse: Surgery. Voices for PFD. https://www.voicesforpfd.org/pelvic-organ-prolapse/surgery/
- (n.d.). Pelvic Organ Prolapse: Symptoms and Types. Voices for PFD. https://www.voicesforpfd.org/pelvic-organ-prolapse/symptoms-types/
- Gupta, P., Payne, J., Killinger, K. A., Ehlert, M., Bartley, J., Gilleran, J., Boura, J. A., & Sirls, L. T. (2016). Analysis of changes in sexual function in women undergoing pelvic organ prolapse repair with abdominal or vaginal approaches. International urogynecology journal, 27(12), 1919–1924. https://doi.org/10.1007/s00192-016-3066-9
- (n.d.). Pessaries. Voices for PFD. https://www.voicesforpfd.org/about/pessaries/
- (n.d.). Physical Therapy. Voices for PFD. https://www.voicesforpfd.org/about/physical-therapy/
- Culligan, P. J., Lewis, C., Priestley, J., & Mushonga, N. (2020). Long-Term Outcomes of Robotic-Assisted Laparoscopic Sacrocolpopexy Using Lightweight Y-Mesh. Female pelvic medicine & reconstructive surgery, 26(3), 202–206. https://doi.org/10.1097/SPV.0000000000000788