Stress Urinary Incontinence
Relief from leaks
is possible
Approximately 78 million women in the U.S. suffer from urinary incontinence1 and of those, over 37% had Stress Urinary Incontinence (SUI).
Are you living with Stress Urinary Incontinence?
The muscles in your urethra work like a valve, opening and closing as needed to let urine out. But with stress urinary incontinence, also called SUI, the pelvic muscles that normally support the bladder and the urethra are weakened.
When this happens, urine leaks out of the bladder and can leave you feeling embarrassed, frustrated and unsure of what is happening to you.
Symptoms of stress urinary incontinence
Do you leak during any of the following activities?:
- Laughing
- Coughing
- Sneezing
- Heavy lifting
- Physical activity
- Sex
If you can say “yes” to one or more, you should talk to a doctor who is familiar with SUI and discuss a more permanent solution for treating urine leakage.
Find your path to incontinence relief
No two people walk the same path to a diagnosis or a solution. Every woman’s experience with stress urinary incontinence (SUI) is different, and they may reach these steps at different paces and during different stages in their lives.
The right doctor will listen to you and put your needs first. But how do you find them?

Find out more about post-op downtime and what to expect after heading home.


What causes SUI?
SUI can slowly develop as you age and may also be the result of a specific event such as childbirth, or be a result of smoking, obesity or other previous tissue traumas in the area.2
What are your treatment options?
You name it, you’ve tried it. From pads, diapers, special underwear and Kegels – some of it helps, but doesn’t relieve the burden of SUI. You deserve a treatment that addresses the source of the problem, not something that just provides a temporary fix for symptoms.
Learn more about a lasting solution for SUI below.

Avoiding and covering up leaks only adds to the burden of having SUI in the first place. A lasting solution, with minimal downtime, can help relieve the added burden of constantly hiding your SUI symptoms.
Luckily, there’s Altis® Single Incision Sling.
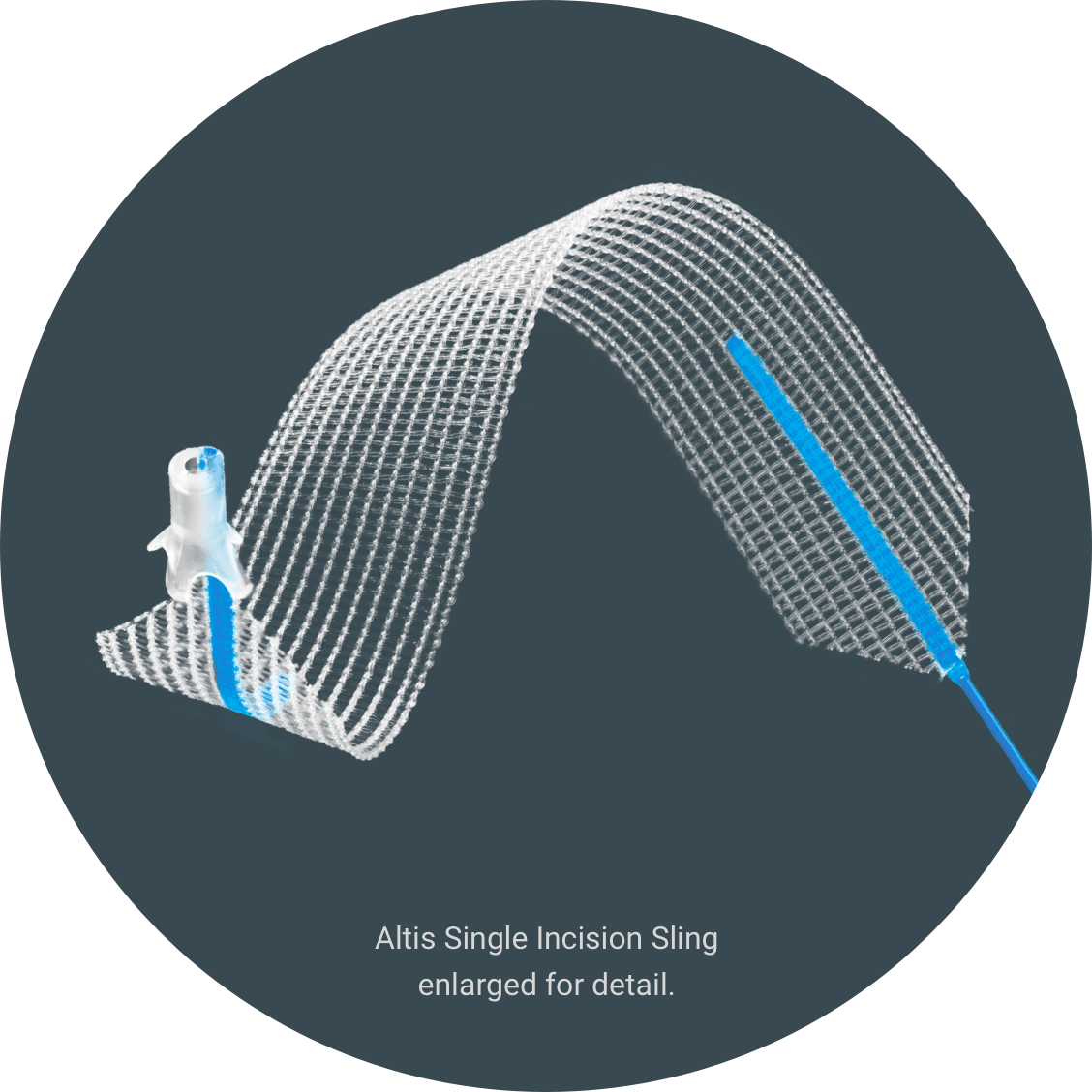
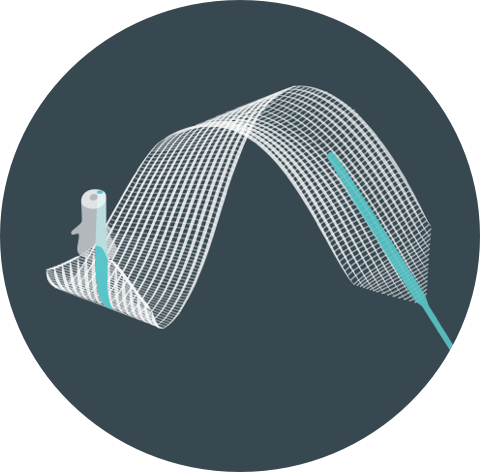
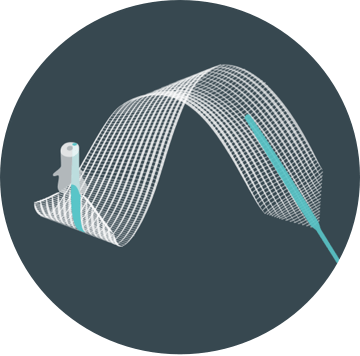
Introducing Altis®
Women experiencing SUI deserve a clinically proven, effective solution. Altis is a treatment backed by clinical studies with firsthand testimonials from women who’ve had the procedure with successful outcomes.
Altis is a sling that treats stress urinary incontinence by supporting the urethra to keep it in its correct position.3 The procedure is a minimally invasive4 outpatient surgery.3
What have others experienced?
0 %
saw a median reduction in pad weight5
0 %
reported feeling “very much better” or “much better” improvements after their surgery at 24 months5
0 %
reported no urine leakage related to SUI at 24-months post procedure5